Karl F. Kothbauer
Pediatr Neurosurg (2007) 43 (3): 236–248
1. Introduction
Tethered cord syndrome (TCS) is a neurological disorder characterized by the abnormal attachment of the spinal cord to the tissues within the spinal canal. This tethering limits the spinal cord’s natural movement, causing stretching, compression, and damage to the nerves over time. TCS can lead to a variety of symptoms, ranging from mild to severe, which may worsen with age or growth spurts in children.
2. Causes
TCS can be caused by both congenital and acquired factors. Congenital factors include spina bifida occulta, split cord malformations, lipomyelomeningocele, and tight filum terminale. Acquired factors involve spinal cord injury, inflammation, infection, or scar tissue formation from previous surgeries. In some cases, the exact cause of TCS remains unknown.
3. Epidemiology
The prevalence of TCS is approximately 1 in 4,000 live births, but this number may be underestimated due to underdiagnosis or misdiagnosis. TCS affects individuals of all ages but is more commonly diagnosed in children and adolescents due to the increased risk of symptom progression during periods of growth.
4. Symptoms
The symptoms of TCS can vary greatly among individuals and may include:
- Back or leg pain, often exacerbated by physical activity or stretching
- Muscle weakness or atrophy in the legs
- Numbness, tingling, or decreased sensation in the lower extremities
- Incoordination or difficulty walking
- Gait abnormalities, such as foot drop or toe walking
- Scoliosis or other spinal deformities
- Bladder or bowel dysfunction, including incontinence or constipation
- Sexual dysfunction, such as erectile dysfunction or infertility
- Lower extremity deformities or contractures
5. Pointers to Diagnosis
The diagnosis of TCS is based on a combination of clinical history, physical examination, and imaging studies. Key elements in the diagnostic process include:
- Detailed patient history, including symptoms, progression, and any relevant family history
- Thorough physical examination, focusing on neurological function, gait, and spinal deformities
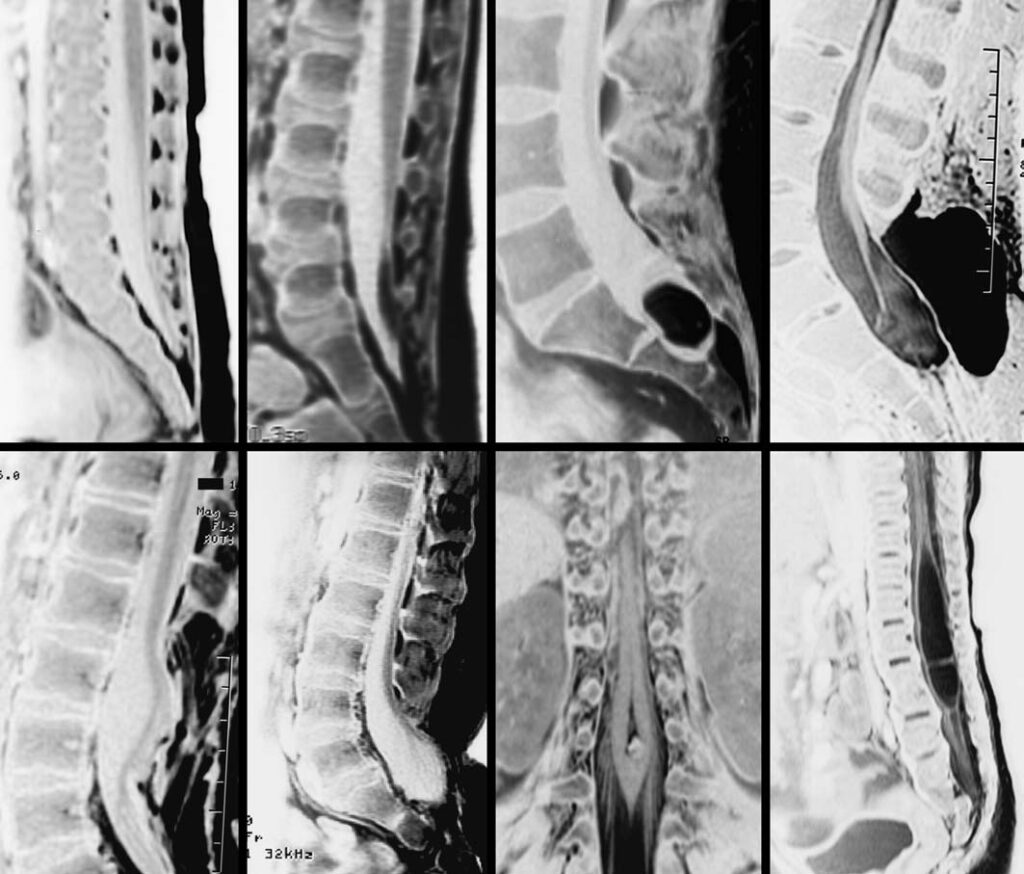
- Imaging studies, such as MRI, to visualize the tethered spinal cord and identify any underlying structural abnormalities
In some cases, additional tests like urodynamic studies, nerve conduction studies, or electromyography may be useful in evaluating the extent of neurological dysfunction
6. Natural History
The natural history of TCS varies widely depending on the cause, severity, and individual factors. Some patients may experience mild, stable symptoms, while others may have progressive neurological deterioration without intervention. The growth spurts in children can exacerbate the stretching of the spinal cord, leading to worsening symptoms or new neurological deficits.
7. Treatment Options
The treatment options for TCS include:
- Conservative management: Pain management, physical therapy, and bladder or bowel dysfunction management, aimed at improving function and quality of life
- Surgical intervention: The primary surgical treatment for TCS is untethering, which involves releasing the tethered spinal cord and correcting any underlying structural abnormalities. In some cases, additional procedures like spinal fusion or decompression may be necessary to address associated spinal deformities or stabilize the spine.
8. Timing of Surgery
The optimal timing for surgery in TCS patients depends on factors such as the patient’s age, the severity and progression of symptoms, and the potential risks and benefits of surgery. Early surgical intervention may be recommended for patients with significant neurological deficits or those at risk of progressive deterioration to prevent irreversible damage.
9. Recovery and Rehabilitation
The recovery and rehabilitation process for TCS patients may involve a multidisciplinary approach, including:
- Physical therapy to improve strength, flexibility, and range of motion
- Occupational therapy to enhance fine motor skills and activities of daily living
- Pain management strategies, such as medications or nerve blocks, to alleviate pain and discomfort
- Bladder and bowel management programs to address incontinence or constipation issues
- Counseling and psychological support to help patients and families cope with the challenges associated with TCS
The duration of the recovery and rehabilitation process varies depending on the individual’s needs and the extent of surgery.
10. Outcome
Outcomes for TCS patients depend on factors such as the severity of the condition, the success of treatment, and the patient’s overall health. Some individuals may experience significant improvement in symptoms and regain a high level of functioning, while others may have residual deficits or complications, such as chronic pain, bladder or bowel dysfunction, or spinal deformities.
11. Follow-up
Regular follow-up is essential for TCS patients to monitor for any changes in symptoms or neurological function. Follow-up visits may include:
- Periodic physical examinations to assess neurological status, gait, and spinal alignment
- Imaging studies, such as MRI, to evaluate the spinal cord and surrounding structures for any new or recurrent tethering
- Additional tests, if needed, to assess bladder or bowel function, nerve conduction, or muscle function
Discussions of any further treatment needs, including potential surgical revisions, if symptoms recur or worsen.
12. Summary
Tethered cord syndrome is a complex neurological condition resulting from the abnormal attachment of the spinal cord within the spinal canal. Diagnosis is based on a combination of clinical history, physical examination, and imaging studies. Treatment options include conservative management and surgical intervention, with the goal of improving the patient’s quality of life and preventing neurological deterioration. Regular follow-up is crucial to monitor for any changes in symptoms or neurological function.
13. Disclaimer
This website provides general information about healthcare topics to help individuals make informed decisions and connect with medical professionals for support. However, it is important to note that the information on this website is not a substitute for professional medical advice, diagnosis, or treatment. It is recommended to always seek the advice of a qualified healthcare provider for any medical questions or concerns. Reliance on any information provided on this website is solely at your own risk. If you are interested in scheduling an appointment with a qualified specialist in Pediatric neurosurgery, you can contact us via phone or message on Telegram / WhatsApp at +91 8109 24 7 365.
