1. Introduction
Chiari malformation is a structural defect in the back of the skull. Children may be born with this malformation, or develop it later in childhood.
There are four types of Chiari malformations. Chiari I and II are the most common types. Chiari III and IV are extremely rare.
Causes of Chiari Malformation
Doctors are not sure what causes Chiari malformations. The defect begins before birth when the base of a baby’s skull does not grow to a normal size. After birth, the skull hardens as the brain grows. This creates a mismatch between the skull size and brain size. As a result, the child’s brainstem, cerebellum and cerebellar tonsils become crowded.
Over time, the cerebellar tonsils (and sometimes the brain stem) get pushed down into the spinal canal. This blocks the flow of cerebrospinal fluid and causes symptoms.
In rare cases, a Chiari malformation occurs later in life to a child whose skull grew normally before birth. This is called acquired or secondary Chiari malformation. Causes can include an injury, exposure to a harmful substance or an infection.
Types of Chiari Malformations
Chiari I occurs when a portion of the brain called the cerebellar tonsils extends out of the skull and into the upper part of the spinal canal. This can disrupt the flow of cerebrospinal fluid. It is a little bit like what happens when a rock is sitting in the middle of a stream.
Chiari I can cause symptoms in infancy. Symptoms sometimes do not occur until late childhood or early adulthood, if at all. This condition often is diagnosed when a person has imaging tests for unrelated reasons.
Chiari II occurs when the cerebellar tonsils and the brain stem push down through the base of the skull into the upper spinal canal. Chiari II is often called Arnold-Chiari malformation. It is present at birth. Typically, it is seen in infants with myelomeningocele (a form of spina bifida) and/or hydrocephalus (a buildup of cerebrospinal fluid in the brain). It is the most common type of Chiari malformation. Almost all children with a myelomingocele have Chiari II malformation.
Chiari III and IV are very rare and may be life-threatening. Please talk to your child’s physician for more information about these diagnoses.
Chiari Malformation Symptoms
A variety of problems can occur with Chiari malformations. Symptoms vary for each child.
Chiari I
The main symptom with Chiari I is a headache in the back of the brain. The headache can be severe. Other problems can include:
- Dizziness and balance problems
- Double or blurred vision
- Numbness
- Spontaneous gagging and vomiting
- Sensitivity to bright lights
In rare cases, a child will experience sleep apnea. This is a condition in which breathing pauses during sleep.
Diagnosing Chiari I in an infant is challenging. Symptoms are not always obvious. Also, the child is not able to communicate exactly what is wrong. Common signs can include irritability, head banging and nighttime wakening.
About half of patients with a Chiari I malformation also develop a syrinx, which is sometimes called a syringomyelia or hydromyelia. A syrinx is a fluid-filled cavity in the spinal cord. It occurs when the normal flow of cerebrospinal fluid is obstructed.
A syrinx expands over time. It can injure nerve fibers in the spinal cord. It eventually can cause symptoms such as:
- Muscle weakness in the extremities
- Muscle stiffness
- Reduced ability to feel pain or temperature
- Chronic pain
- Loss of bladder and bowel control
- Numbness and tingling
- Clumsiness
Chiari II
Chiari II is most often seen in infants with myelomeningocele, a form of spina bifida. Symptoms can include swallowing problems and slow or noisy breathing. The condition can lead to feeding problems, gagging, drooling and vomiting.
Conditions Associated with Chiari Malformation
Children with a Chiari malformation sometimes have associated conditions. For this reason, it is important that they receive care from a multidisciplinary team of physicians. Team members may include doctors who specialize in pediatric neurosurgery, neurology, disorders of the ear, nose and throat, and other areas of medicine.
Conditions Associated with Chiari I
Patients with Chiari I may develop a syrinx, scoliosis, and/or have a tethered spinal cord.
- A syrinx is a fluid-filled cavity in the spinal cord. It can lead to a number of neurological problems. These include muscle stiffness, weakness and pain. Surgeons typically do not operate to correct the syrinx. But surgery to correct the Chiari malformation may relieve these symptoms.
- A syrinx can cause scoliosis, an abnormal curvature of the spine. For some children, treating the Chiari malformation can alter the progression of scoliosis. In other cases, children may need additional surgery to treat the scoliosis itself.
- In rare cases, a child with a Chiari malformation may have a tethered spinal cord. This means that their spinal cord is abnormally attached to tissues around the spine. A child may need surgery to correct the tethered cord, in addition to treatment for the Chiari malformation.
Children with Ehlers-Danlos syndrome (EDS) may be at increased risk for Chiari I malformation. EDS is a connective tissue disorder that causes hypermobility and unstable joints.
Conditions Associated with Chiari II
Two serious conditions associated with Chiari II are myelomeningocele and hydrocephalus. A multidisciplinary team can help diagnose and treat these conditions.
- Myelomeningocele is a severe form of spina bifida. It occurs when part of the spinal cord and surrounding nerves stick out from an opening in the spine. Children with this condition sometimes have other medical problems. These can include hydrocephalus and heart defects.
- Hydrocephalus is a buildup of cerebrospinal fluid in the brain and spinal cord.
In addition, some children with Chiari I or II have some form of sleep apnea. This is a condition in which they stop breathing temporarily during sleep. Treating the Chiari malformation may stop or lessen the sleep apnea.
Diagnosing Chiari Malformation
A magnetic resonance imaging (MRI) test is the best way to detect a Chiari malformation. An MRI can create three-dimensional images of the brain and upper spinal cord from many angles. This helps doctors make an accurate diagnosis.
MRIs also can help physicians see whether the child has a syrinx within the spinal cord or a tethered spinal cord. Follow-up MRIs can help the medical team see whether the Chiari malformation changes or worsens over time.
Once the medical team establishes a diagnosis of Chiari malformation, other tests can be used to help evaluate the child’s condition. These include:
- Computed tomography (CT) scan. This test can show blockage in the spinal canal.
- Ultrasound scan. This test can evaluate motion of the cerebellar tonsils during surgery.
- Evoked potentials. These electrical tests can determine whether the brainstem is functioning properly. They also can give information about peripheral nerves, the spinal cord and brain function.
- A swallowing test. This test can show how well the child is able to drink liquids or swallow thickened food. It is helpful for children who experience gagging or excessive drooling.
- A sleep study. This study can look at a child’s breathing pattern and determine whether enough oxygen is getting to the brain during sleep. This test is helpful for children who have a history of noisy sleeping or snoring.
Chiari Malformation Treatment
Treatment for Chiari I and II varies depending on many factors. These include the exact type of malformation, the progression of the structural defect and the child’s symptoms.
If your child has a syrinx in the spinal cord, the team will recommend decompression surgery. The purpose of this surgery is to relieve pressure on the brain and spinal cord.
Rarely, the medical team may recommend surgery to place a shunt. A shunt is a tube that can help establish a normal flow of cerebrospinal fluid around and behind the cerebellum.
Chiari I Treatment
If your child has Chiari I but does not have a syrinx or symptoms, no treatment is necessary. The medical team will perform follow-up MRI scans to monitor your child’s condition. If the malformation is causing neck pain or headache, pain-relief medication may help. If your child is experiencing swallowing issues, speech therapy may be helpful.
If the pain is severe, or your child is experiencing other symptoms that affect his or her quality of life, the medical team may recommend decompression surgery to relieve symptoms. Without surgery, a child will likely continue to have symptoms, which may worsen over time.
Chiari II Treatment
Children with Chiari II typically do not undergo surgery, unless the malformation is causing breathing and swallowing difficulties. In that case, the medical team may recommend decompression surgery.
Long-Term Outlook
Some children never require treatment for a Chiari malformation. Others are able to enjoy a good quality of life with the help of non-surgical therapies. These therapies may include pain-relief medicine or physical therapy.
When surgery is needed, results are often very positive. Many children are symptom free or have significantly fewer symptoms. Follow-up care includes performing MRIs at regular intervals. These tests help doctors evaluate the results of the decompression, the response of any associated syrinx, and any scar tissue development.
In a small number of cases, a second decompression surgery may be needed.
What is Chiari Malformation Surgery?
For children having symptoms of and who have been diagnosed with Chiari malformations, the treatment is surgery to create more space for the brain and spinal cord. Without surgery, symptoms will continue and may worsen.
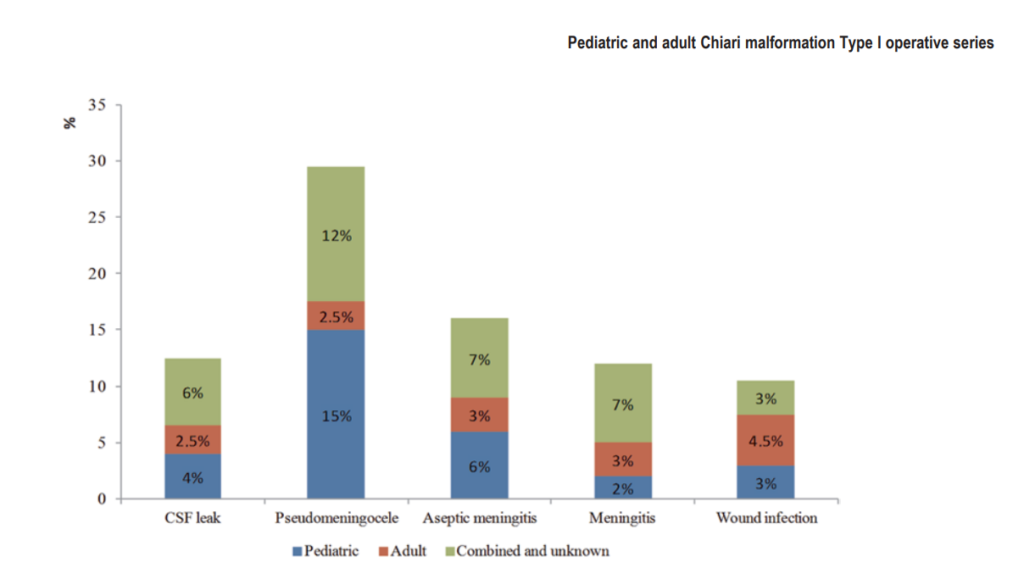
Risks of surgery include excessive bleeding, cerebrospinal fluid leak, infection, no relief of symptoms, paralysis, problems swallowing, abnormal eye movements and anesthesia complications.
The family and the neurosurgeon decide if surgery is the best option.
What Is Decompression Surgery?
Decompression surgery describes a number of different procedures. This type of surgery is used to remove the bone that is compressing the cerebellar tonsils. When successful, this reduces pressure on the brain and spinal cord. It also restores the normal flow of cerebrospinal fluid.
Decompression surgery is performed under general anesthesia.
- First, a small cut is made at the back of the head.
- The muscle is gently moved out of the way.
- A small piece of bone is removed from the bottom of the skull to create the extra space.
During surgery, the surgeon uses imaging technology to view the movement of the cerebellar tonsils and surrounding cerebrospinal fluid. This helps to determine whether the patient will benefit from more extensive decompression. If the space is okay, the surgery is over and the incision is closed.
If more space is needed:
- The surgeon makes a cut in the covering of the brain, called the dura mater.
- The surgeon may need to sew a patch over the opening to keep cerebrospinal fluid from leaking.
- Sometimes, the surgeon may shrink the cerebellar tonsils to make more room for the cerebrospinal fluid to circulate. These tonsils do not have any known purpose.
The surgical technique may vary. If your child has a syrinx or hydrocephalus, he or she may need a tube (shunt) to drain the excess fluid.
Decompression surgery can take two to three hours. Recovery typically includes one night in the intensive care unit and three to four days in the hospital. Your child will experience pain and swelling after surgery. Our team will prescribe medication to make him or her comfortable during the healing process.
After returning home, your child will need to avoid some activities for a couple of months. These include heavy lifting and contact sports. He or she should also avoid anything that causes neck strain, such as carrying a heavy backpack. During follow-up appointments in the clinic, your child’s doctor will provide specific instructions.
Preparing Your Child for Surgery
The hospital offers tours of the surgical facilities several days a week. This program is very helpful for both child and family. Please call 513-636-8298 to make reservations for this educational program.
You will need to do a few things to get your child ready for surgery. A checklist will help make sure you are prepared. View the pre-surgery checklist.
On the day before surgery, a nurse or technologist will take a sample of your child’s blood for a complete assessment. You will need to have this done at the test referral center located at the main hospital or at one of the satellite facilities. The test referral center’s hours of operation are 7 am-8:30 pm Monday through Friday and 8:30 am-4:30 pm Saturday. If you have questions, call the test referral center, 513-636-4461.
If your child’s neurosurgeon has told you that your child will need a blood transfusion for surgery, you have the option of using the blood provided through Hoxworth Blood Center or donating through Hoxworth’s Directed Donor Program.
Blood obtained through regular donations is as safe as blood secured through directed donors. This is especially true if the directed donor is not the parent or immediate relative. Women who have given birth within the past six months cannot donate blood. If you are interested in the Directed Donor program, call Hoxworth at 513-451-0910 or 1-800-830-1091.
To help prepare for a successful surgery, share with us your child’s full medical history. Please report:
- Any bleeding disorders within the family
- Any medications the child is currently taking, including vitamins and herbal or natural supplements
- Any medication allergies
Tell us if your child has a known allergy to latex. Any unexplained problems with surgery, watery eyes, sneezing or wheezing while playing with balloons may be due to a latex allergy. Anyone who has had multiple surgical procedures might have such an allergy.
Day of Surgery
On the morning of surgery, wash your child’s head with tear-free baby shampoo and then rinse your child’s scalp thoroughly.
Arrive at the hospital two hours before the scheduled time of surgery and bring your child’s overnight bag, the form completed by your child’s pediatrician and your insurance card. If you plan on spending the night with your child while he or she recovers with us, remember to bring your own overnight bag.
A doctor called an anesthesiologist will talk with you about methods of pain control appropriate to your child’s size and age. This doctor will also ask you about your child’s past anesthetics as well as family reactions to general anesthesia. Be prepared to provide this information; it is very important in preventing possible reactions to anesthetic agents that may be used during the surgery.
During the Surgery
The surgery is performed under general anesthesia. The length of surgery is specific for each patient, and you will be updated often during the surgery.
After the Surgery
Your child will spend at least four to six nights with us following surgery. When your child is able to eat regular food well and meets other discharge goals, he or she can go home. Children usually return to full, normal activity in 12 to 14 days. Refer to any of the following sections if you have concerns once you and your child get home.
Pain Management
Please give acetaminophen regular children’s Tylenol as directed for your child’s pain. If the pain is not relieved with acetaminophen, you may give your child oxycodone.
Wound Care
Please wash your child’s incision each day using the neurosurgery wound wash kit which includes baby shampoo and sponges.
Activity After Surgery
For several days after surgery, your child will not feel like being active. Activity should be limited to quiet play for the first week after leaving the hospital. Further activity instructions will be given at your first postoperative visit.
Bathing After Surgery
Your child should shower with mild baby soap or shampoo daily. A sponge bath with mild soap followed by rinsing with clean water is fine for smaller children. Do not allow the wound to soak in the bathtub.
Call Your Child’s Doctor If:
Call the doctor, 513-636-4726, if you are concerned with your child’s progress after surgery or if your child experiences:
- Temperature greater than 102° F
- Bleeding or drainage from the incision
- Confusion or excessive sleepiness
- Severe headache that does not stop with Tylenol and rest
- Excessive vomiting
