Craniosynostosis,
Pediatric Neurology,
Volume 53, Issue 5,
2015,
Pages 394-401,
ISSN 0887-8994
1. Introduction
Craniosynostosis is a congenital condition characterized by the premature fusion of one or more of the cranial sutures, the fibrous joints that connect the bones of the skull. This can result in abnormal skull growth and shape, leading to potential issues with brain development and function. Craniosynostosis can be classified as either isolated (occurring without any other associated abnormalities) or syndromic (associated with specific genetic syndromes). Early diagnosis and intervention are crucial for optimal outcomes.
2. Causes
Craniosynostosis can occur due to various factors, including:
Genetic factors: Certain genetic mutations or syndromes, such as Apert, Crouzon, or Pfeiffer syndrome, can increase the risk of craniosynostosis.
Environmental factors: Some studies suggest that certain maternal factors, such as smoking or drug use during pregnancy, may contribute to the development of craniosynostosis.
Idiopathic: In many cases, the exact cause of craniosynostosis remains unknown.
3. Epidemiology
Craniosynostosis affects approximately 1 in 2,500 live births, with some variations depending on the type of suture fusion and presence of associated syndromes. Males are more likely to be affected than females, with a ratio of around 1.6:1.
4. Symptoms
The primary symptom of craniosynostosis is an abnormally shaped skull. Other symptoms may include:
- A visible ridge along the affected suture
- Asymmetry in the shape of the head or face
- Slower or faster head growth compared to body growth
- Increased intracranial pressure, which can cause headaches, vomiting, irritability, and vision problems in severe cases
- Developmental delays, particularly if brain growth is restricted
5. Pointers to Diagnosis
Diagnosing craniosynostosis typically involves the following steps:
Medical history and physical examination: A healthcare provider will assess the child’s symptoms, examine their head and face, and inquire about family history.
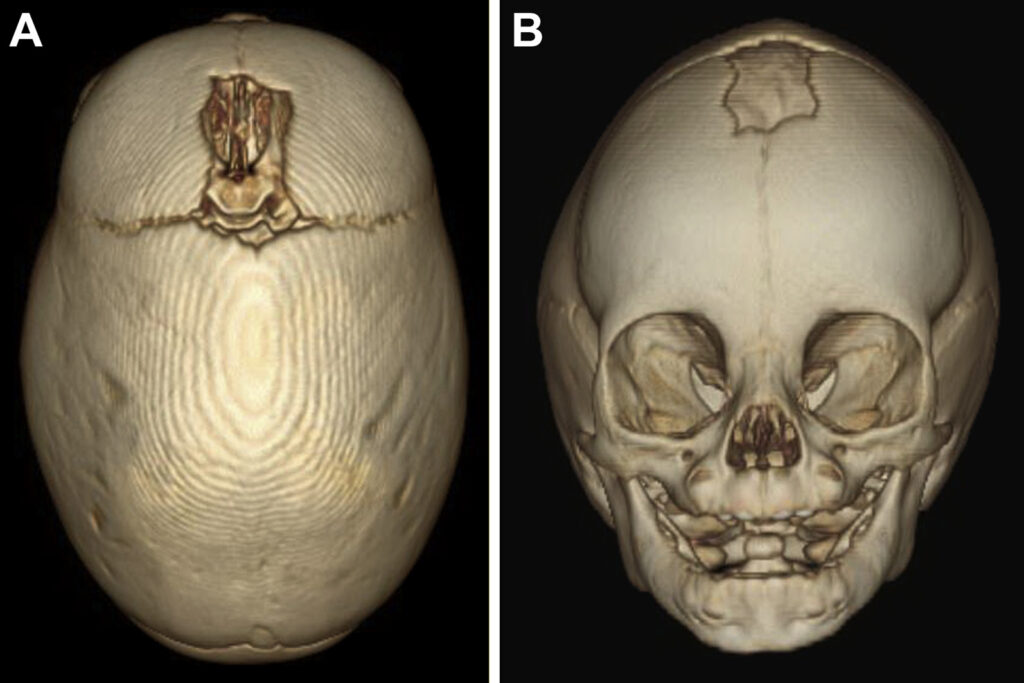
Imaging studies: X-rays, Ultrasound scans, CT scans, and MRI scans can be used to confirm the diagnosis, visualize the affected sutures, and evaluate any underlying brain abnormalities.
6. Natural History
If left untreated, craniosynostosis can result in various complications, including:
- Abnormal head and facial appearance
- Increased intracranial pressure and potential brain damage
- Vision and hearing problems
- Cognitive and developmental delays
- Social and emotional difficulties due to appearance-related concerns
7. Treatment Options
The primary treatment for craniosynostosis is surgery, which aims to correct the shape of the skull, relieve any pressure on the brain, and create space for normal brain growth. There are two main surgical approaches:
- Open cranial vault reconstruction: This involves removing and reshaping the affected skull bones and repositioning them to allow for normal skull growth.
- Minimally invasive endoscopic surgery: This involves making smaller incisions and using an endoscope to release the fused sutures, followed by the use of a custom-made helmet to help guide the skull’s growth.
The choice of treatment depends on factors such as the child’s age, the severity and type of craniosynostosis, and the presence of any underlying conditions.
8. Timing of Surgery
The timing of surgery for craniosynostosis depends on several factors, such as the child’s age, the severity and type of craniosynostosis, and the presence of any underlying conditions. In general, surgery is recommended as early as possible to minimize the risk of complications and promote optimal brain growth. For open cranial vault reconstruction, surgery is typically performed between 6 and 12 months of age. For minimally invasive endoscopic surgery, the procedure isusually performed between 3 and 6 months of age. The specific timing of surgery will be determined by the healthcare team based on the individual needs of the child.
9. Recovery and Rehabilitation
Post-surgery, children typically stay in the hospital for 2-7 days, depending on the type of surgery and the child’s overall health. Pain management, antibiotics, and close monitoring are essential during the recovery period. Children who undergo minimally invasive endoscopic surgery will need to wear a custom-made helmetfor several months to help guide the skull’s growth. This helmet must be worn for 23 hours a day and adjusted regularly by a specialist.
Following discharge from the hospital, regular follow-up appointments with the healthcare team are essential to monitor the child’s progress and ensure proper healing. Some children may require additional surgeries or interventions, such as speech therapy, occupational therapy, or physical therapy, to address any developmental, cognitive, or motor-related issues.
10. Outcome
The outcome for children with craniosynostosis largely depends on the severity of the condition, the timeliness of treatment, and the presence of any associated syndromes or complications. With early diagnosis and appropriate surgical intervention, many children can experience significant improvement in their symptoms and lead fulfilling lives. However, some children may continue to experience developmental delays, cognitive issues, or ongoing medical care related to their condition.
Long-term complications can include scarring, infection, or the need for additional surgeries to address any growth or appearance-related concerns. Support from specialists, such as pediatric neurosurgeons, plastic surgeons, and rehabilitation therapists, is essential to ensure optimal outcomes for children with craniosynostosis.
11. Follow-up
Long-term follow-up and monitoring are crucial for children with craniosynostosis. Regular check-ups with healthcare providers, including pediatric neurosurgeons, plastic surgeons, and neurologists, help ensure proper healing and address any potential complications. Additionally, children with craniosynostosis may require ongoing evaluations and interventions from other specialists, such as occupational therapists, physical therapists, and speech therapists, to address any cognitive, motor, or speech-related issues.
Parents and caregivers play a vital role in supporting children with craniosynostosis, advocating for their needs, and ensuring they receive appropriate care and resources. Support groups and organizations dedicated to craniosynostosis can offer valuable connections and resources for families navigating the challenges of living with the condition.
12. Summary
Craniosynostosis is a complex congenital condition caused by the premature fusion of one or more cranial sutures. Timely diagnosis, surgical intervention, and comprehensive long-term care are crucial for improving outcomes and helping children with craniosynostosis lead more fulfilling lives. By understanding the causes, symptoms, and treatments of craniosynostosis, individuals and their families can better advocate for their care and manage the challenges associated with this condition.
13. Disclaimer
This article provides general information about healthcare topics to help individuals make informed decisions and connect with medical professionals for support. However, it is important to note that the information in this article is not a substitute for professional medical advice, diagnosis, or treatment. It is recommended to always seek the advice of a qualified healthcare provider for any medical questions or concerns. Reliance on any information provided in this article is solely at your own risk. If you are interested in scheduling an appointment with a qualified specialist in Pediatric neurosurgery, you can contact us via phone or message on Telegram / WhatsApp at +91 8109 24 7 365.
